Warning – medical details – do not read if you are squeamish about such things!
I saw Mr. Pullan, my colorectal surgeon, today, as a follow-up after my recent CT scan which confirmed my suspicion that my parastomal hernia had returned. This is one of the images from the CT scan, which I annotated – it clearly shows the hernia.
This hernia has now been repaired twice, and last time I saw Mr. Pullan, in August, he said that if I was correct and the hernia had returned, it would be more difficult to repair this time because a) it had already been repaired twice and b) there was now a Permacol biological mesh in place.
Today, having seen the scan images, he was able to enter into a more constructive discussion of options. He didn’t have the images in front of him so I showed him this one on my iPad and he was fascinated by the annotations! He found it useful as he was able to point out various things, including the considerable size of the defect through which the hernia is emerging.
He said first of all that (as I already knew), the next step in such cases was to re-site the stoma on the other side of the abdomen, because repeated repairs weaken the surrounding muscle and any further repair along the same lines would be less likely to be effective. I reminded him also of the fact that during the hernia repair operation he had made extra incisions either side of the stoma to give him more room to manoeuvre which would have further weakened the area, and he agreed with this. We also agreed that we were starting from a disadvantage from the outset, because my muscles are already very weak due to my ME.
I told him I really didn’t want to go down the moving-the-stoma route, which he understood and appreciated – I said that Kermit, my stoma, is working fine, and I am used to him being where he is, and surely moving him would just introduce another site for potential herniation, which he agreed would be the case. He said that also, there was a lot more “plumbing” involved with moving an ileostomy to the left-hand side of the abdomen – ileostomies are always on the right because this is where the junction between the small and large intestines is, so it is logical to place the stoma here when the colon is removed. Colostomies, on the other hand, are always sited on the left, and lower down, for the same reasons of anatomy. Moving the stoma would mean starting from scratch again with a brand new stoma and all its associated problems – although of course I now have quite a bit of experience under my belt (literally!) and I wouldn’t be dealing with these as a newbie, and would know how to cope with it all. I told him that since the last repair operation in March of this year when he inserted the mesh, I have had no trouble with Kermit because as I requested, Mr. Pullan made him longer so the output tends to go into the bag rather than underneath it. Previously he had been retracting flush with the skin and causing a lot of leaks and skin irritation. During this operation, Mr. Pullan inserted the mesh through the hole in the abdominal wall through which Kermit emerges, remaking him in the process, thus avoiding open surgery again, which I have already had done twice. Kermit is now a much better shape than previously, causing everything to work a lot better, and I am reluctant to disturb this state of affairs.
I asked him what were the pros and cons of simply leaving things as they were. He had told me after my first repair operation in January 2017 that smaller hernias were more likely to cause obstructions than larger ones. That operation was an emergency, following an obstruction caused by the first hernia which was quite small, and could easily become restricted. I asked him how large the hernia is now, in terms of risk of obstruction. He said it was medium-sized, so I suppose it carries medium risk of obstruction. He said that having experienced one before, I knew the signs, and would know what to do. I told him I knew that obstructions were a call for an emergency visit to A&E and that they were life-threatening, and that if there was nothing in the bag and I was throwing up, I would go straight away. He said that that was good, but it could be in a dangerous state even if I had not started vomiting, and if I noticed any change from normal, such as pain in that area, I should be on high alert and seek immediate advice.
My hubby said that if we just left it alone, it might cause another obstruction, necessitating emergency surgery again, for which I was not prepared, and in an already weakened and compromised condition, leading to a less favourable outcome as far as recovery was concerned. I said I agreed with this, but having elective surgery also carries risks – after all, my repair operation in March of this year led to a serious, life-threatening infection.
Turning to the possibility of further surgical intervention, he said this was quite a problem. It’s not just the fact that it’s been done before and there is now mesh in place, but the position of the hernia is an issue, being in the right iliac fossa, where there are quite a few structures in a relatively small space – the most difficult site for a parastomal hernia. Each time it has recurred in the same place. He examined me again, and remarked that I am quite short in the body and there isn’t a lot of space between the bottom of my rib-cage and the top of my pelvis, which makes this situation worse. I suggested six months of spinal traction to stretch me but he laughed and didn’t think that would really help!! (Might be nice to be a few inches taller, though…)
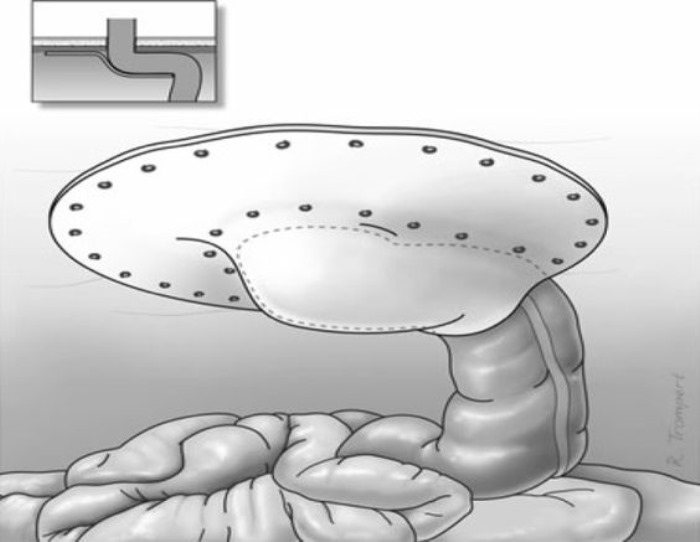
He said there were various alternative surgical approaches to repair intractable parastomal hernias, including a procedure known as the Sugarbaker technique. I told him I knew about this, having done some research prior to my last repair. It involves attaching a piece of mesh to the inside of the abdominal wall, and rather than cutting a hole in the mesh through which the end of the intestine passes in order to form the stoma, the mesh is applied over a length of bowel, forming a tunnel over it, trapping it against the inside of the abdominal wall and preventing it from moving around and emerging through any defect in the muscle. There is some risk involved in anchoring a section of bowel in this way as the loops of intestine are designed to slide over one another with the passage of food, and it can cause a blockage. He said that he had not performed this operation but the literature was positive about its outcome. When I got home I did some further research on this, and found that compared with other forms of repair (simple suturing – 100% recurrence – this is what I had for the first repair, performed as an emergency following an obstruction, performed by a general surgeon not qualified to perform a better repair at that time, and “keyhole” repair, where a hole is cut in the mesh, through which the stoma passes – a slightly better prognosis but still resulting in fairly high percentages of recurrence – this is the type of repair I had in March of this year), Sugarbaker has a much lower rate of recurrence and is more likely to remain stable. Statistics vary, of course, depending on a variety of factors, such as the length of time spent monitoring for failure post-operatively in the various trials, and differences in individual patients, such as age, weight, lifestyle etc.
Here is a diagram of mesh attached using the Sugarbaker technique.
I said I was fairly reluctant to face further surgery if it could be avoided, especially in view of how ill I was after the last operation, and he understood this. We agreed that it was a matter of weighing the risks of further surgery and doing nothing, which could result in another obstruction and the necessity for emergency surgery with all the disadvantages of that – for example, no proper physical and emotional preparation, which can adversely affect the outcome with slower recovery times etc. Also, as happened to me before, by the time they eventually did operate, I had been vomiting and not eating for several days (waiting from the Sunday morning till Tuesday evening for a CT scan!!) and was in a seriously weakened state which is not ideal for someone about to undergo major surgery.
We spoke a bit about my post-operative experience this year, being readmitted a fortnight after discharge with a severe infection. He recalled the further operation required to insert the larger and deeper of the two drains, I told him how much pain the larger drain had caused, especially when it was first moved, and then removed – about the worst pain I had ever experienced – and we talked about my brief stay in Mum’s nursing home on discharge, not just to help me convalesce, but also for my hubby’s benefit. I said that I had felt so poorly with the infection, and he agreed that I had been very seriously ill.
I said I did not relish the risk of a repetition of that, and I asked what was the cause of the abdominal haematomas that gave rise to the infection. He said that I had probably been put back on the rivaroxaban (anticoagulant) a bit too soon after surgery, and if there had been something weakened that had bled a little, under normal circumstances this would have healed up on its own, but in my case, the reduced clotting of the blood had caused more extensive internal bleeding. In such cases, the body launches a defence in the form of an invasion of macrophages to mop up the bleed, and the whole thing can get very sludgy and infected. It was a relief to know that there was a logical reason for the internal bleed and that it was not likely to happen again.
He also said that the internal bleeding itself could ultimately have led to the failure of the hernia repair. It could cause the mesh not to adhere correctly, leading to an early return of the hernia. The biological mesh would eventually be absorbed by the body without having done its job. I found this explanation for the failure of the repair quite fascinating, and it did explain a lot. Initially I was amazed and disappointed that the mesh repair had failed so rapidly, and couldn’t understand why this should have happened.
Mr. Pullan said he would like to consult a colleague at the Royal Devon and Exeter Hospital (RD&E) and run some of his thoughts past him to see if he could come up with any other ideas of how to deal with this intractable problem, and to weigh up the risks and benefits of various approaches. He would send him my scan images and full details of everything that had been done to me so far, and he may or may not want to see me himself. He is probably one of the colorectal surgeons from that hospital who came to speak to our local Ileostomy Association about parastomal hernias soon after my original operation – it seemed to be an area of particular interest to him. It would be strange if it was the same surgeon – unfortunately I can’t remember his name.
I really appreciate all the trouble Mr. Pullan is taking, and the thought he is putting into my case – I have been very impressed with this aspect of my relationship with him throughout. He is a very thoughtful and thorough man, and he is always very open with his ideas and suggestions, keeping me fully informed, and all the while listening carefully to my own views and opinions, and answering all my questions in a considerate and informative way. I always come away having learnt something interesting. I have always taken a great interest in all aspects of my various medical conditions and their treatment, and have taken a lively interest in everything done to me and for me, and I have found that everyone associated with my care has responded very well to this, and have been more than willing to explain and discuss in depth any issues of interest to me. Probably the majority of patients just go in, have stuff done to them and leave, happy to remain in blissful ignorance, but that’s not enough for me! I find the whole thing fascinating, and this attitude seems to be appreciated as most of them love their work, and enjoy talking about it. I love to hear of the latest advances etc. and how the professionals are working at the cutting edge (sometimes literally!) for our benefit. We are so blessed to have such consummate professionals to care for us in our wonderful NHS, especially when they are as charming and personable as Mr. Pullan and those others who have been involved in my treatment and care. Hats off to them all!
I came away from the appointment with answers to questions I had not even thought to ask. It was a very constructive and informative consultation and an educational experience. We now await further developments.
I was also able to have a word with the stoma nurse about the ongoing saga of the support pants. Having heard nothing further from the company for a while, I phoned the rep yesterday and left a message on her voicemail, asking for a progress report on the final pants that I am still waiting for. I have two pairs, and can just about manage with those, but I will be stuck if I have an accident – I need one on, one in the wash, and a spare in case of emergencies. She said she would email them today and ask them what was going on, and to contact me asap. She said it was very poor that I had had to wait over three months to get even the first pair. I said the trouble was, they had no competition as they are the only company that does both home visits and a bespoke service, and she said lack of competition should make no difference, and the way things had been dealt with was not good enough. She did add, though, that when they got it right, the garments were excellent, and I had to agree with her. The two pairs I have got are really good – a very good fit, beautifully made, and they do what they are supposed to do, too.
So we await further developments on that front, too.


OH, my friend! I'm so sorry you are going thru' all of this! I totally understand your reticence about having another surgery as I have an umbilical hernia, as well as ME, like you may remember. Mine has gotten larger but my GP agreed to just watch it. Any problems and she'll send me to a surgeon to watch it! I just want it to disappear! (Mine came originally as I'd had laparoscopy surgery years ago and the area was weak. Doing crunches popped it out!) I feel for you and wish you didn't have to go thru' all of this. I'm hoping for the best outcome for you! Hugs from across the pond! ♥
ReplyDeleteVery interesting Shoshi, I’m like you, very proactive in everything in respect to my medical condition a research ask questions and I believe Good d gave us our Bodie and made our brains as we needed them to survive. I honestly believe it has kept me alive because of learning to handle a very complex condition.
ReplyDeleteGod will bring you and hubby safely through this trial, as He works through wise folk overseeing your needs.
Lack of pants not grand, frustrating plus.
Xxx